Could Losing Sleep Break Hearts?
The Link Between Sleep Apnea and Cardiovascular Disease
- By Carla Saavedra
- Jun 01, 2009
 Fifteen years ago, John Barrera began to notice he felt tired during the day. "I figured it was old age creeping up on me," he says. His snoring became notoriously loud, disrupting his entire household and sometimes waking him up at night.
Fifteen years ago, John Barrera began to notice he felt tired during the day. "I figured it was old age creeping up on me," he says. His snoring became notoriously loud, disrupting his entire household and sometimes waking him up at night.
Eventually, taking naps at lunch was the only way Barrera could make it through the day. After a year of constant badgering from his wife and son, he went to see his doctor. The doctor ran some tests, and Barrera found out his bellowing snore was an indicator of a bigger problem: obstructive sleep apnea (OSA).
Untreated sleep apnea results in more than just lost sleep, however. Studies have shown that the condition does a number on the heart as well. Barrera was lucky. He had not yet developed cardiovascular disease when he was diagnosed, but that's not the case for many people with OSA.
"Sleep apnea can cause heart problems or make existing heart problems more difficult to manage and more dangerous," says Dr. Alejandro Chediak, medical director of the Miami Sleep Disorders Center, immediate past president of the American Academy of Sleep Medicine and associate professor of medicine at the University of Miami.
More than 18 million American adults have obstructive sleep apnea, according to the National Sleep Foundation. Although the link between sleep apnea and cardiovascular problems is well known, recent studies have shed light on just how harmful untreated sleep apnea can be to the heart.
A Physical Toll
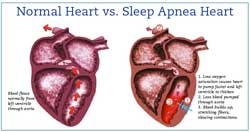
Sleep apnea first affects the heart at the cellular level. A 2006 Antwerp, Belgium, study on the cardiovascular effects of sleep apnea found that patients with OSA had low levels of oxygen saturation in their blood at night, causing the heart to pump faster and the left ventricle to become thicker.
"If I took a 10-pound weight in my right hand and started doing curls, initially my right bicep would get bigger," explains Ron Riley, RRT, registered vascular technologist (RVT), Cardiovascular Visions, Ponca City, Okla. "If I continue to curl that weight for a long time, eventually my muscle would wear out and start to fail."
If what is causing the left ventricle to bulk up is left untreated, Riley says, the organ begins to thin out and fail. And the thinner it is, the less the ejection fraction — the percentage of blood pumped out of a ventricle with each heartbeat. The excess liquid eventually stretches out the fibers used to contract the ventricle.
Riley compares the process to overstretching a rubber band. "Each individual cell has a stretch factor, but if you overfill or overthicken those cells, they lose the ability to shorten effectively," he says.
The same study discovered that 40 to 80 percent of stroke patients had obstructive sleep apnea. A different study, presented at the American Thoracic Society International Conference in 2005, showed that people with obstructive sleep apnea were three to four times more likely to have a stroke in four years than those without sleep apnea. One reason for stroke risk may be that sleep apnea can lead to higher blood pressure. Sleep fragmentation caused by the disorder increases the reactivity of blood vessels, causing them to constrict more and relax less. The surface of the vessels then becomes stickier, which leads to a higher risk of clots and can contribute to the formation of coronary occlusion and myocardial infarction.
"All of those things set up the vascular system of the human for easier occlusion, more blood pressure problems, more problems controlling blood sugar and lipids," Chediak says. "Those are the kinds of things that then create a chronic change in the blood vessel walls and facilitate strokes and heart attacks."
Patients with congestive heart failure can develop central sleep apnea. Unlike obstructive sleep apnea, in which breathing is inhibited by a physical obstruction, central sleep apnea occurs when the brain does not send a signal to the lungs to breathe.
Because some congestive heart failure patients have increased levels of carbon dioxide in their blood, they often develop an abnormal breathing pattern called Cheyne-Stokes respiration. This breathing pattern results when the brain is forced to regulate the extra carbon dioxide. Essentially, the brain ignores the oxygen level in the lungs and instead monitors the carbon dioxide levels in the blood to determine when to breathe. Signals also slow down. Patients breathe more rapidly to respond to the build-up of carbon dioxide. Once the rapid breathing thins the carbon dioxide, breathing slows down or stops until carbon dioxide levels rise again. With Cheyne-Stokes, patients exhibit repetitive cycles of rapid breathing followed by slow breathing or apnea, which becomes dangerous when a person is sleeping.
Patients with central sleep apnea can be vastly different from those with obstructive sleep apnea. "Patients look different, they complain about different things, and they respond differently to therapy," Chediak says.
CPAP Reversal
Fortunately, continuous positive airway pressure (CPAP) therapy can improve and even reverse some of the adverse effects of sleep apnea on the heart. Co-morbidities, such as blood pressure and hypertension, that have become drug-resistant in sleep apnea patients are alleviated with CPAP treatment.
"A patient that suffers from pulmonary hypertension and is resistive to drugs they are on, treating the sleep apnea can bring the hypertension down to normal levels or levels that can be treated with CPAP therapy along with drug therapy," says Greg Dunn, respiratory manager, Alpine Home Medical, Salt Lake City, Utah. He says sometimes the changes are drastic.
"I am very amazed at some of the patients that come into the store in a wheelchair or have limited mobility," Dunn says. "They get on the therapy, we educate them and months later, they come in walking."
A patient's apnea/hypopnea index (AHI) is the best indicator of how effective treatment will be. "The people who have the worst apnea/hypopnea indexes are the people who benefit the most," Riley says, explaining that people with an AHI of 42 or higher will drop to the lower 20s after being on CPAP therapy.
"Those that have Cheyne-Stokes, if you treat them with a bi-level, they drop into the 4 range," Riley says.
Although patients with central sleep apnea greatly benefit from CPAP therapy, it is more difficult for a sleep lab technician to titrate and adjust the device based on a person's breathing in one night.
"If you bring a patient with Cheyne-Stokes or central sleep apnea into the sleep laboratory and try to (titrate), you're going to go nuts because the central sleep apnea does not respond acutely, it responds over time," Chediak says. If a technician doesn't understand the differences between the apneas, he or she may increase the pressure to where it's unbearable for the patient, he says. Moreover, central sleep apnea patients may require additional treatments, such as supplemental oxygen.
Chediak says that respiratory therapists have to take extra care of congestive heart failure patients because they are more delicate. "These are patients that have a pretty far advanced heart dysfunction and failure, and so respiratory therapists have to be more cognizant of the fact that they're going to be on more drugs," Chediak says. These patients may not be able to handle CPAP pressures and may be more suited for auto PAP, he says.
Bi-level devices are a good alternative to CPAPs if a patient can't handle higher pressures. "But we always want to use the less-is-more approach," Riley says. For most patients, a CPAP works just fine.
A Cheyne-Stokes breather who is apneic for a long period of time, however, will need a bi-level device to keep the patient breathing, Riley says.
Teaching Compliance
Although positive airway pressure therapy is the ticket to controlling and improving cardiovascular co-morbidities, patient compliance is a huge issue among the sleep apnea population. Barrera's hesitance to get tested is only one of many barriers patients have to receiving proper therapy — just using a CPAP requires an adjustment.
"The CPAP has a humidifier that takes some experimenting with to get to your comfort level," Barrera says. "But I have noticed a difference in my energy during the workday. I don't really look forward to a nap anymore, so I try to do more reading."
The first few weeks are the most difficult for patients as they adjust to the CPAP's pressure. Respiratory therapists can play an important role in helping patients stick with therapy. Educating the patient about treatment, ameliorating common misconceptions and emphasizing an improved quality of life encourages patients to stick with the therapy.
Choosing the right equipment also is an integral part of patient compliance. Chediak says that making little changes, such as using a different mask, less tubing or a different device, to make a patient more comfortable will ultimately lead to better compliance.
"If you have a bearded man with a mustache, a mask that has to seal on the mustache may not be the best idea," Chediak says. "Respiratory therapists need to work with patients on things they may not anticipate."
Dunn says it's important for respiratory therapists to emphasize the consequences of discontinuing treatment.
"Say, 'Yes, this is going to be a transition, this is a bit of a cumbersome device, but if you want to see your children's children growing up, then you need to wear this device.' "
This article originally appeared in the Respiratory Management June 2009 issue of HME Business.