Winning at Compliance
Improving CPAP Usage for Trouble Patients
- By Elisha Bury
- Jun 01, 2009
 Despite its documented therapeutic benefit, CPAP therapy has always had some inherent risks when it comes to patient compliance. Some patients find it hard to get used to the constant pressure and to using the CPAP device. Others complain about the noise, fit and comfort of the CPAP mask. Still others worry about the stigma of using the mask in front of others. Sadly, many give up on therapy within the first 30 days.
Despite its documented therapeutic benefit, CPAP therapy has always had some inherent risks when it comes to patient compliance. Some patients find it hard to get used to the constant pressure and to using the CPAP device. Others complain about the noise, fit and comfort of the CPAP mask. Still others worry about the stigma of using the mask in front of others. Sadly, many give up on therapy within the first 30 days.
The struggle to achieve patient compliance is not a new one for respiratory HME providers and therapists. For that reason, compliance has always been top of mind. In fact, many HME companies have established intricate follow-up strategies, and manufacturers are offering more interface options for improved comfort than ever before.
In late 2008, the DME MAC jurisdictions released new local coverage determinations (LCDs) that established a regulation for proving CPAP compliance. The policies mandated a 12-week trial period to show patient benefit for CPAP coverage to continue. Compliance was defined as a minimum of four hours per night, 70 percent of the time in a 30-day period.
Along with that definition came other requirements that created challenges for respiratory providers. “When the PAP LCD was released, the 90-day face-to-face physician visit to establish compliance was troublesome at best,” says Bob Hoffman, president of Nationwide Respiratory, Waterloo, Iowa. “It put the burden on the provider to ensure the patient actually followed through with the physician appointment or risk non-payment. Both the physician and the patient needed to be educated as to why the follow-up appointment was necessary and the ramifications should the visit not take place.”
Now that providers are five months into the new policy (at press time), Respiratory Management wanted to know: How are providers faring?
The Follow-up Visit Hurdle
Hoffman says the first thing most providers did was send letters to physicians explaining the new policy and the necessity of the 90-day follow-up visit. Patients also received similar information and were warned that failure to comply would result in the equipment being picked up or an out-of-pocket expense to continue therapy. Enter problem No. 1.
“The patient often feels it is an unnecessary doctor visit, which creates an inconvenience as well as a financial burden if they do not have co-insurance,” Hoffman says. “Some physicians simply do not agree with the requirement and blame the provider, who is only the messenger, for having to comply with more bureaucratic red tape. We have also heard that the patient feels the physician is requiring the visit, and the patient resists complying because they feel it is an unnecessary office call.”
Medical Service Co., an HME company in Cleveland, Ohio, has encountered a few troubles with some physicians. Patrick Clevidence, vice president of respiratory services, says that most physicians are compliant once they understand what has to be done, but when his company is the first HME to explain the extra requirements, it can be a problem.
“You hate to be the only DME company actually asking for that information,” Clevidence says. “Then you become a little bit more difficult to be referred to. You’re trying to educate the physician and the referral source on what we need without disrupting the referral process. It’s a tight rope.”
Clevidence says the sales force can be instrumental in smoothing the transition. The sales representative has to do a good job of explaining the requirements and showing supporting documentation from Medicare.
Hoffman says that no matter how stringent the follow-up and education protocol is, most providers are having trouble with the physician visit. “It all comes down to the patient driving to the physician,” he says. “If this does not occur, for whatever reason, the provider is forced to discontinue service or make other financial arrangements.”
Clevidence’s team put into place protocols to help prevent missed appointments. “The therapists themselves try to schedule the appointment with the physician at the time they’re doing the setup,” he says. “Then we try to time that with where we think the patient might be. We give them a couple of months to be on the machine, and then we try to schedule picking up the card (and) downloading that information. That way, the physician will have that information when they do their face to face.”
At Oxygen One in Waukesha, Wis., Rebecca Olson, RRT, director of patient care, says getting patients invested in the process requires the provider to thoroughly explain that Medicare requires the follow-up visit and therapy compliance. “Whenever we get you set up, we’ll let you know when you need to follow up with your physician. Have you already made the appointment? We’ve got specific questions we ask,” Olson says. “You set the stage from that first contact with the patient of what Medicare is going to expect from them. It’s not Oxygen One expecting it. Medicare requires you, as their beneficiary, to do (these things) in the first 90 days.”
Gretchen Jezerc, director of U.S. marketing, sleep-disordered breathing, Philips Respironics, Murrysville, Pa., says the key challenge is that more action is required from all of the stakeholders involved in the process. “Essentially you have to have buy-in and involvement and some investment in the process by the patient particularly to actually go to this follow-up visit and by the physician to conduct the visit and share the information back with the DME company,” she says.
From a logistical standpoint, Clevidence agrees. He says it’s getting all of the pieces to work that has been the biggest challenge. “The therapist can schedule the patient to go in and then you have to make sure and hope and pray that the card, we actually receive it back. Then thirdly, that the patient is actually compliant. And then the patient actually shows up for the face to face,” he says. “There are so many pieces involved.”
Compliance Basics
Ensuring that patients meet the compliance requirement means ensuring that patients are comfortable using the device.
“If people have the ability, they should watch their patients closely,” Olson says. “When (patients) get that 21 out of 30 days, (providers) need to get them flipped, get them moving, get them into the doc. It’s a matter of being proactive. Instead of waiting until the denial comes or the patient fails, find out earlier in the treatment, why is this patient struggling? Why is this patient failing?”
Oftentimes, the biggest hurdle to compliance lies with the interface. “A key to compliance is finding a mask that works for the patient,” says Drew Terry, senior director of product management for sleep, ResMed, Poway, Calif. “Each individual patient has a unique face and unique preferences.”
For this reason, it’s important that providers invest in a variety of mask options. Then ask patients key questions: Is the pressure too high? Are patients struggling to find a comfortable sleeping position with the mask? Are they getting excessive leak?
“There are lots of things that you can do once you’ve identified the patients who are having trouble, analyze the data and then have a conversation with the patient to find out where they’re having the challenges,” Terry says. For example, switching to a bi-level device or changing the interface — either to pillows for a more comfortable position or to full-face to stop leak — could make all of the difference.
Olson says that bi-level devices are an option for patients that can’t get compliant. “Within the first 90 days, if they’re failing CPAP, you can switch them to (a bi-level device) and go to 120 days if there’s less than 30 days left in the first 90.”
One of the biggest obstacles to CPAP compliance is that patients fail to understand the consequences of forgoing therapy. “It just takes a lot of time to help people understand the impact of wearing the CPAP vs. if they don’t wear it, the complications that can happen to them even years down the road,” Clevidence says. “It could contribute to congestive heart failure, diabetes, different problems depending on their history.” He says respiratory therapists must be proactive in explaining these consequences.
Clevidence says that sometimes it’s harder for older patients, i.e. the Medicare population, to adjust to CPAP, which makes compliance harder to achieve. “They’ve (seniors) been this way their entire life, and to all of a sudden have to wear this apparatus takes a little bit more time to be comfortable with it I think,” he says.
Another problem many CPAP users face is disturbing the bed partner. Devices and masks with high noise levels may awaken the patient and anyone sleeping next to the patient. “If the bed partner isn’t happy, then the patient isn’t happy either,” Terry says. This problem may require equipment that produces less noise.
Masoud Vahidi, OSA product manager at Fisher & Paykel Healthcare, Irvine, Calif., suggests utilizing CPAP support groups to encourage patient compliance. “Continuous patient education and support is the key for meeting current guidelines,” he says. “Implementing a solid patient follow-up program as well as having the appropriate product that fits patients’ needs is crucial.”
The Technology Question
One strategy for meeting compliance requirements is choosing the proper technology to make proving compliance as easy as possible. But with better technology comes greater financial investment.
Medical Service employed a data card to handle Medicare patients after the new LCD was issued. Clevidence says the added expense was a concern. “But we thought it was the most concrete proof of actually having a hard copy of the data vs. the other option — people could just get the hours,” he says. “We felt that if Medicare ever did an audit, it’s a little bit dicey because in the initial CPAP LCD, it did say you needed to have something that was more substantial than just a call-in. We thought, well, we’ll defer back to that.”
The added expense might be worth it in the long run, however. Kristin Mastin, director of marketing, DeVilbiss Healthcare, Somerset, Pa., says technology assists providers with this laborious and time-intensive process. “It is important that providers review all the technology that is out there today to assist with monitoring the patient and their CPAP usage,” she says. Mastin says technology that allows providers to see the moment a patient has met the CPAP LCD requirements will help optimize efficiencies.
Another benefit of tracking technology is that some software allows providers to sort data so that they can see which patients are struggling with compliance. Then providers can focus their attention on following up with those patients and working toward compliance solutions. “It really makes sense to focus efforts,” Terry says. “If you think about managing 100 patients or 200 patients and trying to get them compliant, it seems like a pretty daunting task. But if you’re able to focus in on the ones that are having the challenges, then it becomes a much more manageable problem.”
Oxygen One implemented a wireless patient management system in March 2008, well before the new guidelines were issued. “We did not see this coming back in March of last year,” she says. “Little did we know that (the system) was going to be a huge saving grace for us come November when Medicare switched things up. By then, we already had the system down. It was just a matter of instead of 30 days, it’s one of two things: compliant or 90 days, whichever comes first.”
The change came about because the company wanted to grow its CPAP business to be clinically sound in terms of efficacy. Oxygen One also wanted to cut out manual follow-up for CPAP patients. “Our philosophy is it’s fine if you put the patient on the equipment, but if the device is not working for them and maintaining clinical efficacy, you need to do something about it,” Olson says.
With the patient management system in place, Olson’s clinical assistant can check each patient daily to see who’s faltering. Then, the assistant calls the patient.
Oxygen One has not had a single Medicare patient fail to meet the new compliance regulations.
Strategies That Work
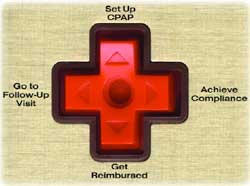
If you’re struggling to make the CPAP compliance requirements work with your patients and referrals, here are some surefire ways to get your business back in order:
1. Communicate with referral sources and patients about the consequences of not meeting Medicare’s requirements. Hoffman recommends that providers inform referral sources of the new requirements either in a letter or by phone — or both. Additionally, providers must thoroughly explain the Medicare guidelines to the client at the time of CPAP setup, he says. Inform the patient that the 90-day follow-up visit with the physician must take place or Medicare will not cover the equipment and supplies. When it comes time for the compliance follow-up call, use that as another opportunity to ask when the physician’s appointment is scheduled and update the patient’s file, Hoffman says. Then follow up with the physician’s office for the results.
2. Educate the patient. “The majority of our installs are here at the office, and they’re a good 45 minutes of education on the disease process and probably 45 minutes instruction on the equipment,” Olson says. “We take our time with the patients. If a patient needs more time, we give it to them.” She says that providers cannot over communicate the new policy.
Olson recommends making the requirements as easy to understand as possible. “We strip it down to just two basic lines: You’re going to have to follow up with your physician. And then they have certain compliance criteria that you’ll need to meet,” she says. That information is repeated each time the company has contact with the patient.
3. Use an ABN. The Advanced Beneficiary Notice (ABN) could come in handy for new PAP patients, says Vahidi. Simply advise patients in advance that if they fail to meet compliance guidelines, Medicare will deny coverage, thereby requiring the patient to be financially responsible for the equipment.
Providers who are nervous about using an ABN might consider following Olson’s lead. “Information on paper is powerful,” she says. To educate patients and remind clinicians to thoroughly explain the Medicare requirements, Oxygen One created a form that outlines what Medicare’s guidelines are and that if the patient does not meet those requirements how much the patient is responsible for out of pocket. The patient then signs the document. Sounds like an ABN, right? It’s not a legally binding document. Olson uses the form strictly as an education tool. “The only reason we have Medicare patients sign it is that they are acknowledging that they understand it,” she says. “They’re repeating it back to me.”
Be sure to consider what’s best for your business before choosing what form to use. Olson says that if she had 15-25 percent of her patients failing, she might consider doing an ABN.
4. Lessen the referral’s workload. Vahidi recommends that providers focus on increasing cooperation with referrals to “further build relationships with physicians’ offices to find ways to lessen the burden on the office staff while getting the required documentation in place.” The less the physician has to do, the more willing he or she will be to get the provider the necessary documentation.
“We shouldn’t expect the physicians to know the hoops we have to jump through to satisfy Medicare,” Olson says. “They’ve got their own hoops. It’s our responsibility to make the physician or referral source’s… job as easy as possible by giving them the education they need to help make our jobs possible.” To accomplish this, Oxygen One asks patients to come back to the office once they reach compliance. At that time, Olson gives the patient a form to take to their physician that outlines what the physician must do, including telling the provider what he or she wants to do regarding therapy and providing a copy of the clinical notes. Physicians “don’t need to remember it because the next patient that comes up, they’ve got the letter to take with them,” she says.
Olson also notifies the physician’s office once the patient is set up so that the office can set the follow-up appointment at that time. “Between the patient knowing they need to go and the doctor knowing they need to come in, we usually end up not even in the process,” she says.
5. Choose the right compliance tracking technology. Because Medicare has wavered with what is necessary to prove compliance, Clevidence recommends that providers err on the side of caution. The benefit of doing this, he says, is that physicians get more information about their patients, which provides them with a better understanding of how patients are doing.
Olson cautions providers that Medicare made it clear that they plan to audit CPAPs. Because of that, she says hour meters just won’t cut it.
While cost is a consideration, Jezerc says, “The reality is that you as a provider will no longer be reimbursed for the majority of your patients whether they are compliant or not. It now depends on being able to both achieve and document compliance.” In other words, choose the technology that works best for your business.
6. Tweak the compliance program you already have in place. Medical Service has had a compliance program in place for years, but the new LCD required a few tweaks. The biggest change has been adding new tracking technology, but the follow-up that occurs on a specific timeline has continued. “With our Medicare patients, with the information we have to gather, it’s just more labor-intensive,” he says. “We have more people involved, and it’s definitely more time consuming, for less reimbursement.”
The follow-up is even more important with the new LCD. “The key is to identify problems early on so that there is still time to intervene, troubleshoot and coach the patient through the acclimation phase,” Mastin says. She says those first two weeks are essential.
Olson didn’t have to change too much with her program. Adding forms to make sure everyone was on the same page did help. Those forms include one explaining to the patient what his or her responsibilities are and another one outlining what physicians must provide from the follow-up visit. Oxygen One also had to adjust equipment expectations: instead of 30 days, the monitoring equipment might be out for 90 days.
7. Assign specific duties to staff members. To keep the process moving, it’s important that all employees involved in CPAP therapy have a clear role. For example, Medical Service’s sales force is clinically astute and therefore does a good job of communicating the new requirements to the physicians and other referrals, according to Clevidence. The respiratory staff at Medical Service also has stepped up its management of patients and collects a lot more information. RTs must work harder with patients who are unable to meet the compliance regulation. Clevidence says his company has established a CPAP clinical coordinator position to manage data, call patients and keep everything flowing. “Any of the things that could go wrong, she intercedes and tries to get it corrected,” Clevidence says.
8. Organize your CPAP program. Clevidence says the most important thing a provider can do is make sure the program is organized. “Make sure you dot every ‘i’ and cross every ‘t’ because it does get to be a lot to handle,” he says. “You have to utilize your staff and prioritize to make sure things are done appropriately or you’re going to find out that six months down the road you have X number of patients that aren’t compliant with no reimbursement to pay for the RT’s time. Who’s going to manage these patients?”
Ultimately, Clevidence has mixed feelings about the new LCD. “It holds companies that didn’t have compliance programs to a higher level,” he says. “But I think it penalizes companies that do have a strong compliance program and a good track record. In some respects, I think it has added cost to our program. In a declining market of reimbursement, that’s difficult. I just wish (CMS) could spend a day in the life of a therapist to see what a therapist does... I think CMS would be really surprised that these aren’t just products that are being put out. There are actual services that require hours of work and follow up for a patient to succeed in their sleep therapy.”
Provider Perspective
“You have to utilize your staff and prioritize to make sure things are done appropriately or you’re going to find out that six months down the road you have X number of patients that aren’t compliant with no reimbursement to pay for the RT’s time.”
—Patrick Clevidence, Medical Service Co.
“If people have the ability, they should watch their patients closely. When (patients) get that 21 out of 30 days, (providers) need to get them flipped, get them moving, get them into the doc. It’s a matter of being proactive. Instead of waiting until the denial comes or the patient fails, find out earlier in the treatment, why is this patient struggling? Why is this patient failing?”
—Rebecca Olson, Oxygen One
Want to talk about Olson’s strategy? E-mail her.
This article originally appeared in the Respiratory Management June 2009 issue of HME Business.